Reducing maternal and child mortality
Fewer women and babies are dying during pregnancy, childbirth, and soon after than ever before recorded. But both Sub-Saharan Africa and South Asia have some way to go to reduce the deaths of mothers to fewer than 70 deaths per 100,000 live births (target 3.1) and neonatal mortality to fewer than 12 per 1,000 live births (target 3.2; figure 3a). In these two regions only half the births were attended by skilled health staff, far fewer than the nearly 90 percent or more elsewhere across the globe. Fewer pregnancies would reduce the number of maternal deaths, but more than 50 percent of married women in low-income countries report that their demand for family planning is not satisfied by modern contraceptive methods.
Ending the epidemics of AIDS, tuberculosis, and malaria
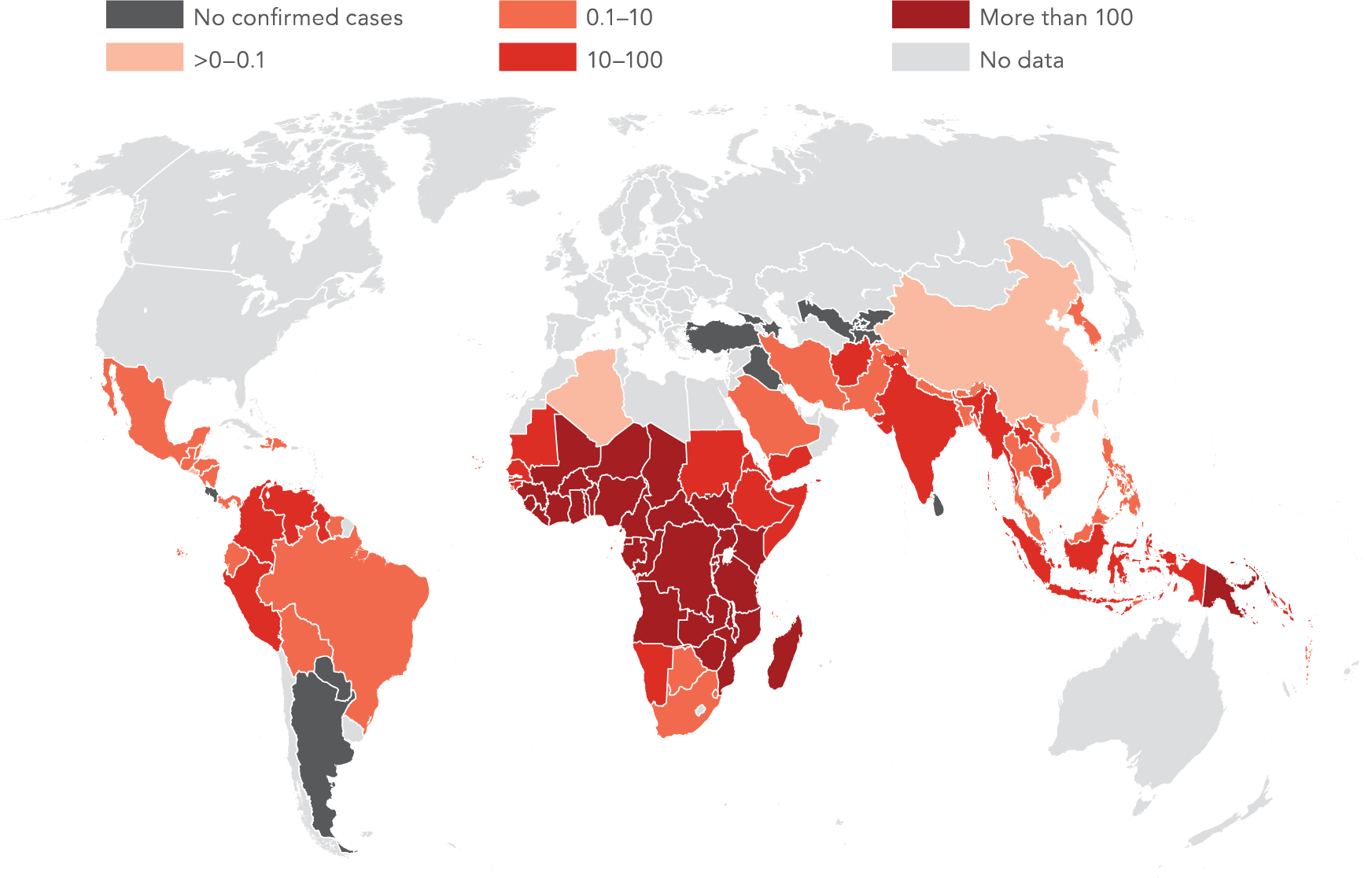
AIDS, tuberculosis, and malaria together affect hundreds of millions of people worldwide, and putting an end to these diseases is a priority under Goal 3 (target 3.3). While the incidence of HIV infection has been declining globally since 1995, the disease is still prevalent in Sub-Saharan Africa, where 3 of every 1,000 uninfected people ages 15–49 contracted it in 2015 (figure 3b). The number of people living with HIV, now at more than 36 million globally, continues to rise since access to antiretroviral therapy increases survival rates.1
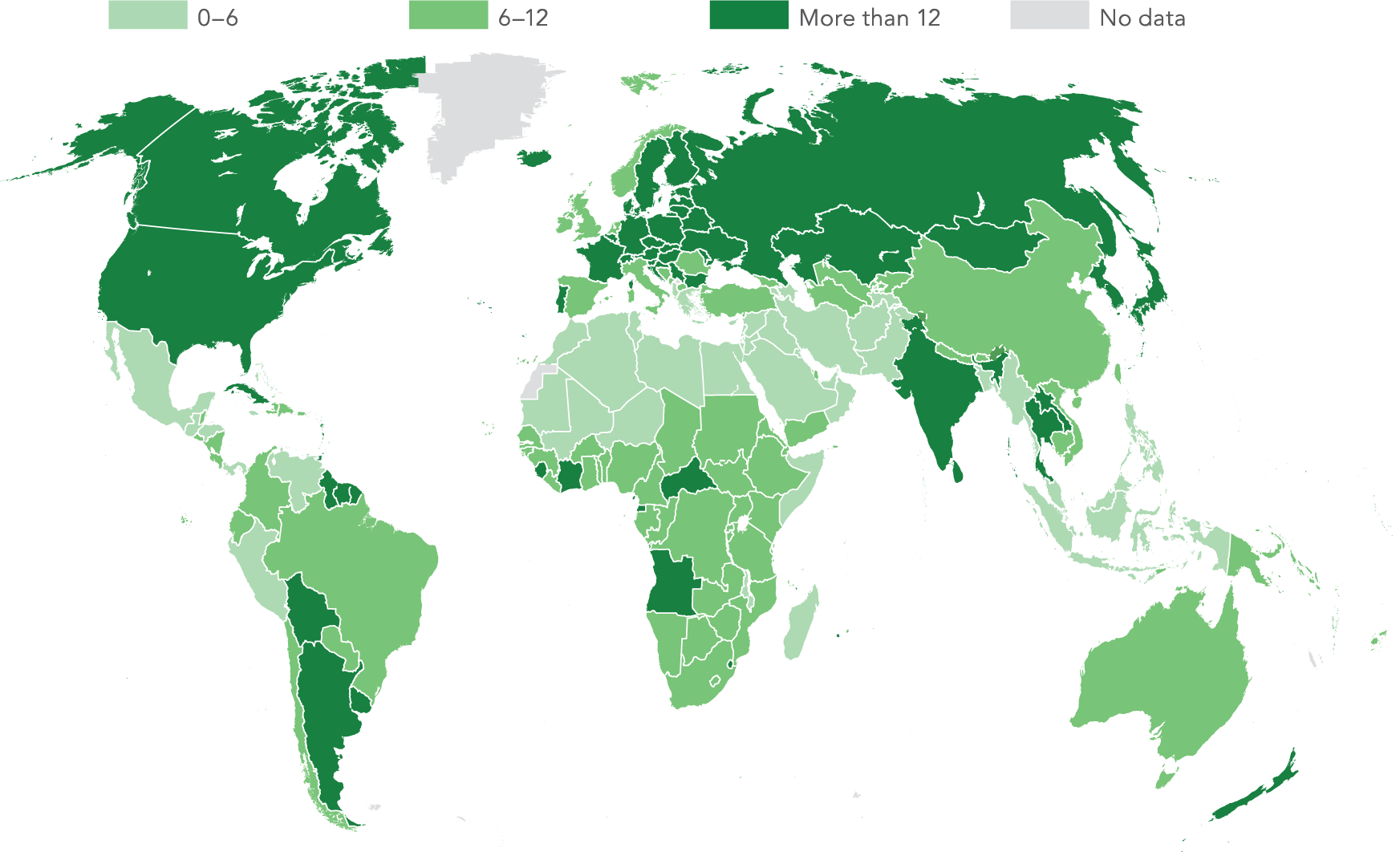
The incidence of tuberculosis, also declining since the early 2000s, remains a global health challenge, especially in Sub-Saharan Africa (276 new cases per 100,000 people in 2015) and South Asia (220; figure 3c). Worldwide there were 10.4 million new tuberculosis cases and 1.4 million deaths due to tuberculosis in 2015.2
Tackling premature mortality from noncommunicable diseases and suicide
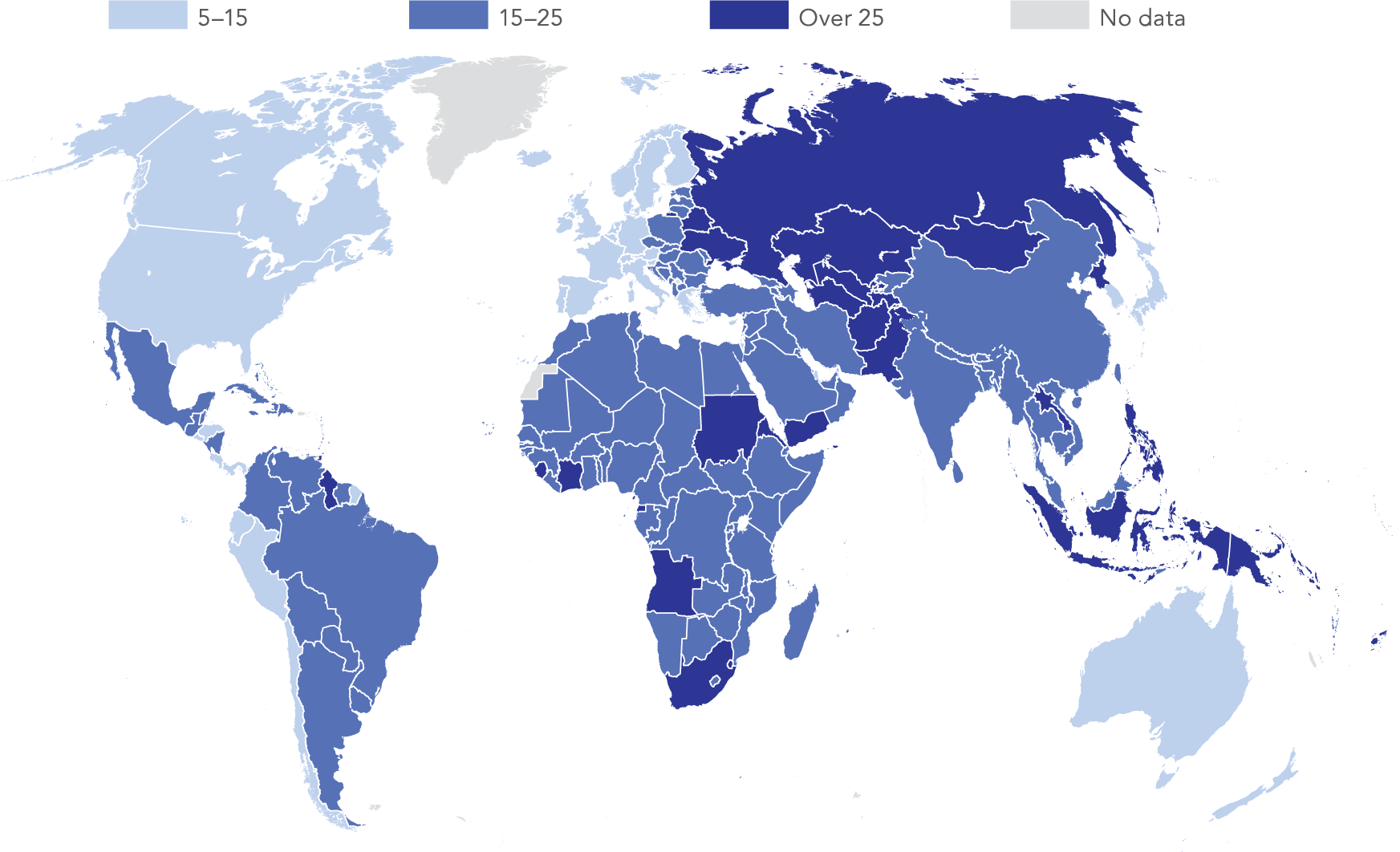
As the incidence of, and deaths from, communicable diseases such as malaria and tuberculosis fall, the share of deaths from noncommunicable diseases increases. Globally, premature death (before age 70) caused by the four major noncommunicable diseases—cardiovascular disease, cancer, diabetes, and chronic respiratory disease—declined 16 percent between 2000 and 2015. To reduce it by one-third by 2030 requires accelerating the current trend (target 3.4). Nine of the 12 highest national rates in 2015 were in East Asia and Pacific or Europe and Central Asia, with Papua New Guinea the highest, where the probability of 30-year-old people dying from these noncommunicable diseases before their 70th birthday is 36 percent (figure 3e).
Mental health is also a focus of target 3.4. Suicide accounts for 8.2 percent of deaths among young adults ages 15–29 globally and is the second leading cause of death after road traffic injuries for that age group.3 Suicide rates for all ages tend to be higher in Europe and Central Asia and in high-income countries (figure 3f).
Preventing substance abuse
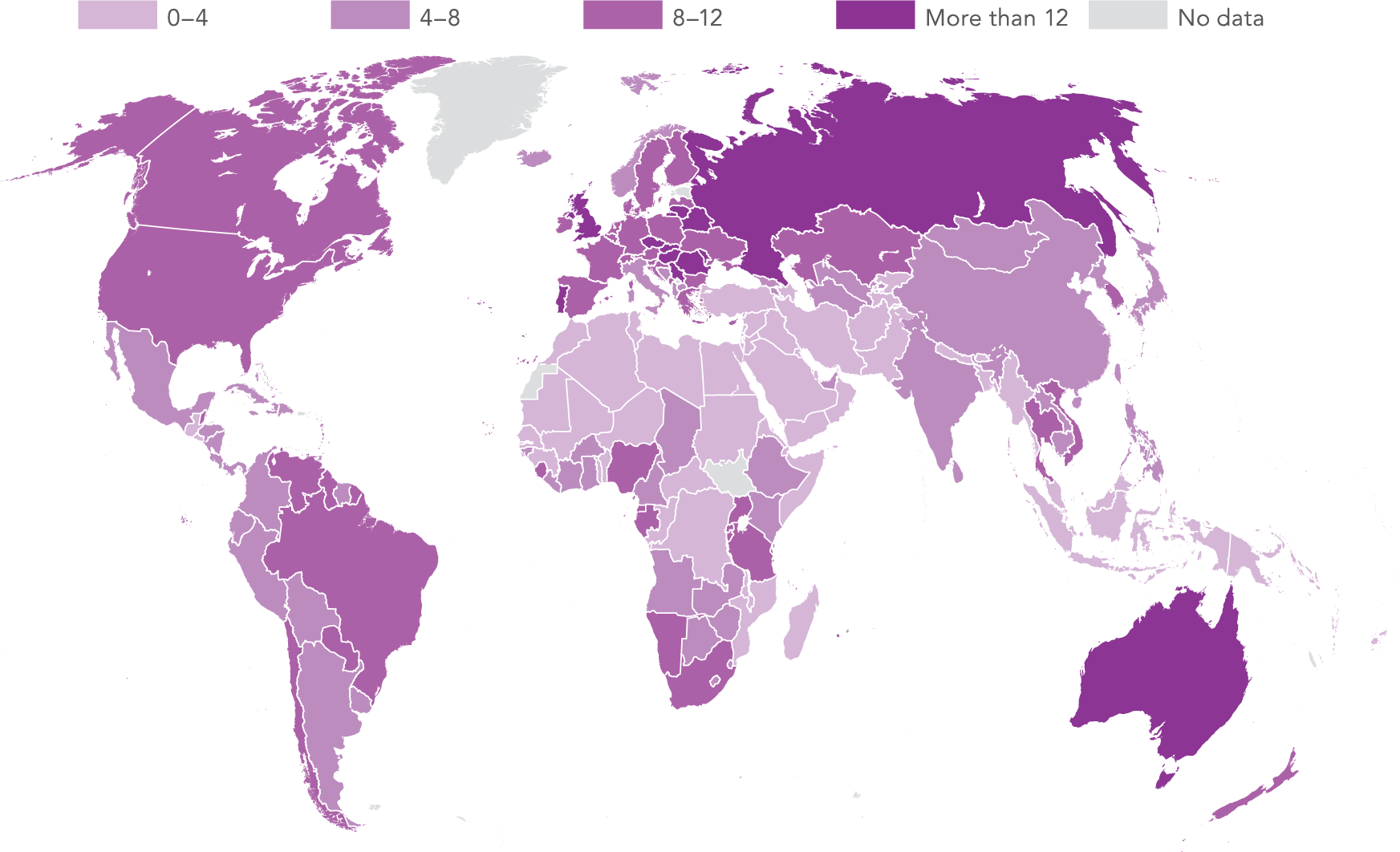
In 2012, 3.3 million deaths—6 percent of deaths worldwide—were attributed to alcohol consumption, predominantly through injuries or noncommunicable diseases.4 Global consumption was 6.3 liters of pure alcohol per person ages 15 and older in 2015, equivalent to 3 liters of beer (4 percent alcohol) a week. Consumption was highest in Europe and Central Asia (10.2 liters of pure alcohol per person a year) and lowest in the Middle East and North Africa (0.8 liters; figure 3g). Goal 3 includes in its agenda preventing and treating harmful use of alcohol (target 3.5).
In 2015 the global incidence of malaria was about 94 per 1,000 persons at risk (figure 3d). Sub-Saharan Africa bears the highest burden, with an incidence of 234 per 1,000 persons at risk. Countries with the highest incidence include Mali (449 per 1,000 persons at risk) and Burkina Faso (389 per 1,000 persons at risk).
Extending financial protection
Universal health coverage strives for people having access to health care without suffering undue financial hardship. Achieving it would prevent people from falling into poverty due to illness and give people the opportunity to lead healthier and more productive lives (target 3.8).
Health care financing in many low- and middle-income countries is still dominated by high out-of-pocket expenditures (figure 3h). Weaknesses in prepayment mechanisms such as taxation or health insurance—and user fees imposed at the point of service—often impede access to care, especially for the poorest.
A meaningful measure of universal coverage needs to reflect the ability of a health system to protect people from the financial risks associated with paying for health care. Universal coverage should offer protection from catastrophic health expenditures—out-of-pocket payments representing a large share of household consumption, usually with a specific threshold. It should also protect people from impoverishing out-of-pocket payments.
The latest available consumption survey data for 110 countries show that in the median country about 7 percent of the population face out-of-pocket payments in excess of 10 percent of their total consumption, including 3 percent for whom health payments represent 15 percent or more of their consumption.5 Every year, 0.74 percent of people are pushed into extreme poverty (living on less than $1.90 a day) by out-of-pocket health payments, and 12 percent of those already below the $1.90 line are driven deeper into poverty. These problems prevail more in countries relying heavily on out-of-pocket payments to fund health care (figure 3i).
Filling the data gaps
Systematically collecting health data is challenging. Even a basic indicator like under-five mortality requires two complete counts, of live births and child deaths by precise age, which are not always available. More complex data, such as cause of death, require even more detailed, complete, and correctly coded information. Civil registration and vital statistics systems to record these life events remain weak in many countries. Only an estimated half or fewer deaths worldwide are registered with cause of death information. In some countries a verbal autopsy (based on interviews with friends and family members) determines the probable cause of out-of-facility deaths, but distinguishing among noncommunicable causes of death using this method remains a challenge.6 Effective monitoring of the Goal 3 targets will require greater investment in such data collection systems.
Notes
- Joint United Nations Programme for HIV/AIDS. 2016. AIDS by the Numbers 2016. Geneva. http://www.unaids.org/en/resources/documents/2016
/AIDS-by-the-numbers.
- World Health Organization. 2016. Global Tuberculosis Report 2016. Geneva. http://who.int/tb
/country/en/.
- World Health Organization. 2016. Global Health Estimates 2015: Deaths by Cause, Age and Sex, by Country and by Region, 2000–2015. Geneva. http://www.who.int/healthinfo/global_burden
_disease/en/.
- World Health Organization. 2014. Global Status Report on Alcohol and Health 2014. Geneva. http://www.who.int/substance_abuse
/publications/global_alcohol_report/en/.
- These 110 countries have more than 80 percent of the world population.
- World Health Organization. 2016. World Health Statistics 2016: Monitoring Health for the SDGs. Geneva. http://who.int/gho/publications
/world_health_statistics/en/.